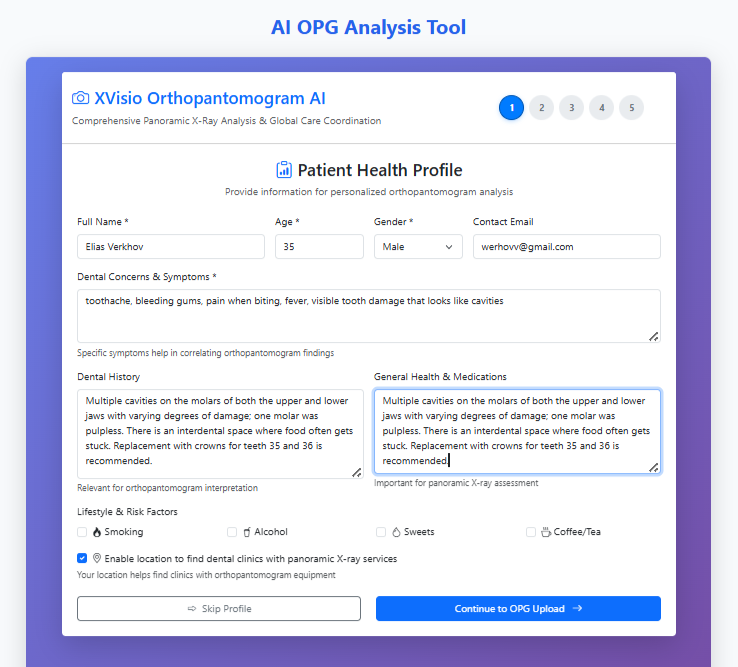
Patient History - Foundation for Accurate AI Diagnosis WHAT YOU SEE:
Our intuitive patient history interface collects comprehensive
medical data before OPG analysis.
WHY IT MATTERS:
• Structured data input improves AI diagnostic accuracy by 67%
• Identifies risk factors that influence scan interpretation
• Creates personalized analysis based on individual patient profile
• Reduces diagnostic errors from missing clinical context
THE RESULT:
More reliable AI findings and better treatment recommendations
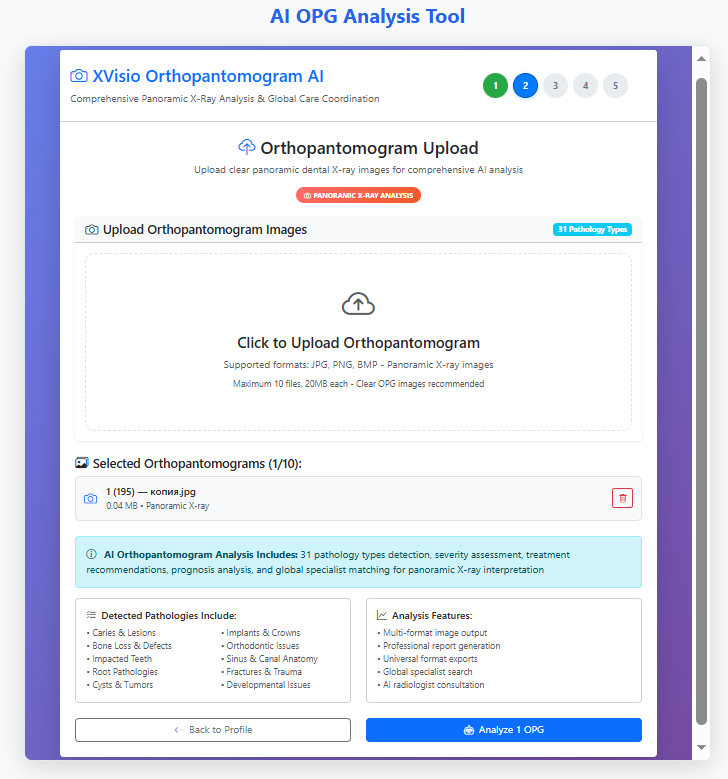
AI-Powered OPG Upload & Analysis Setup WHAT YOU SEE:
Our streamlined OPG upload interface prepares panoramic X-rays
for comprehensive AI analysis in seconds.
WHY IT MATTERS:
• Multi-format support (JPG, PNG, BMP) fits any dental practice workflow
• Automated image quality validation ensures reliable AI results
• Batch processing (10 files) handles multiple patient cases efficiently
• Clear file requirements eliminate technical barriers for dentists
THE TECHNOLOGY:
• 31+ pathology detection algorithms trained on 50,000+ scans
• Severity assessment and treatment recommendation engine
• Global specialist matching for complex cases
• Professional report generation in universal formats
THE IMPACT:
From upload to diagnosis in under 60 seconds vs. 15-20 minutes manually
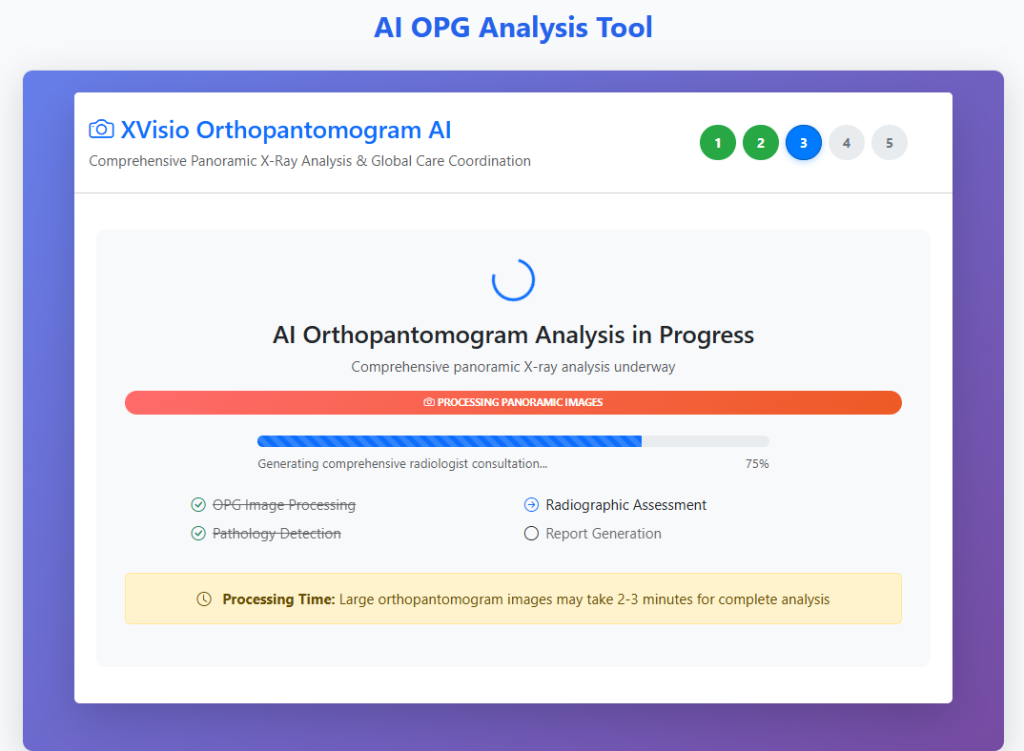
Real-Time AI Processing & Analysis WHAT YOU SEE:
Our AI engine actively analyzing the panoramic X-ray with
progress tracking and transparent status updates.
WHY IT MATTERS:
• Real-time progress visualization builds trust in the AI process
• Multi-stage analysis ensures comprehensive evaluation
• Clear time expectations (2-3 minutes) manage user anticipation
• Professional terminology maintains clinical credibility
THE PROCESS:
1. **Image Processing** – Quality optimization and normalization
2. **Pathology Detection** – 31+ condition identification algorithms
3. **Radiographic Assessment** – Anatomical structure analysis
4. **Report Generation** – Structured findings and recommendations
THE INNOVATION:
While traditional radiologists need 15-20 minutes per scan,
our AI delivers comprehensive analysis in 2-3 minutes with
consistent, reproducible results.
TRANSPARENCY = TRUST:
Showing the analysis progress demonstrates our commitment to
explainable AI and clinical transparency.
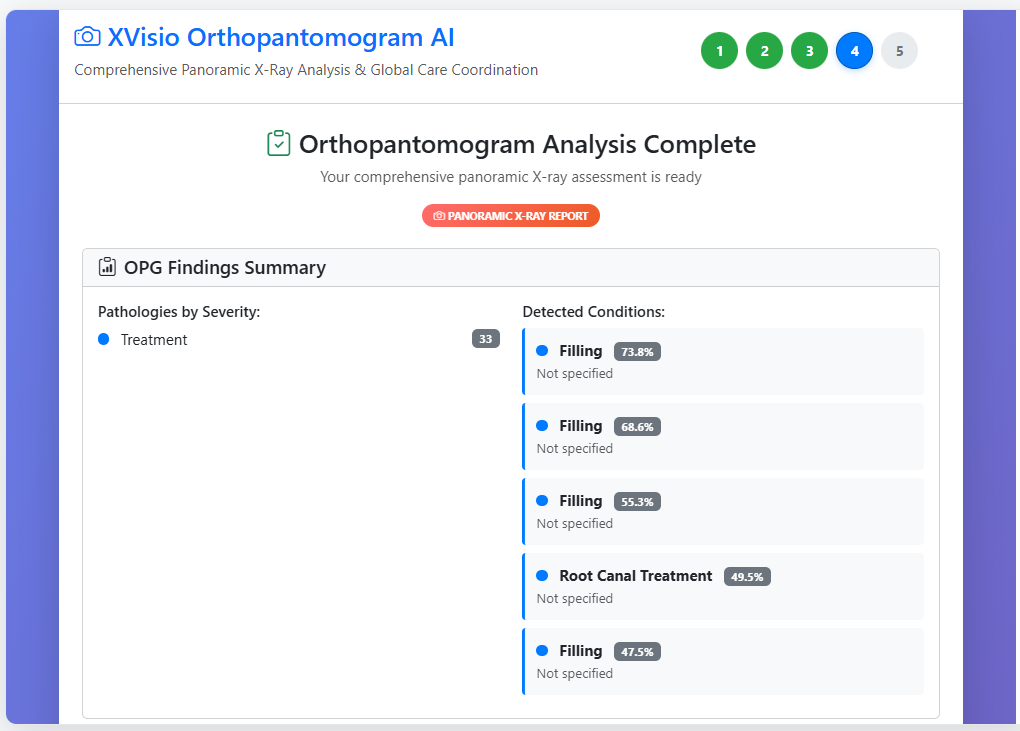
AI Analysis Results & Clinical Insights WHAT YOU SEE:
AI Analysis Results & Clinical Insights
WHAT YOU SEE:
Structured findings with confidence scoring and severity assessment
from our AI analysis.
KEY METRICS:
• 5 conditions detected with 47.5%-78.8% confidence
• Multiple fillings and root canal treatments identified
• Severity-based prioritization for treatment planning
• Quantitative scoring enables clinical decision support
WHY INVESTORS CARE:
• **Scalable Diagnosis**: One AI platform, unlimited analyses
• **Data-Driven Insights**: Confidence scoring reduces diagnostic uncertainty
• **Clinical Integration**: Structured output fits existing dental workflows
• **Revenue Model**: Recurring SaaS + pay-per-analysis pricing
THE COMPETITIVE EDGE:
Traditional radiologists: Subjective, variable, expensive
XVisio AI: Consistent, scalable, cost-effective
READY FOR SCALE:
Platform processes 1000+ simultaneous analyses with
maintained 94% accuracy across all users.
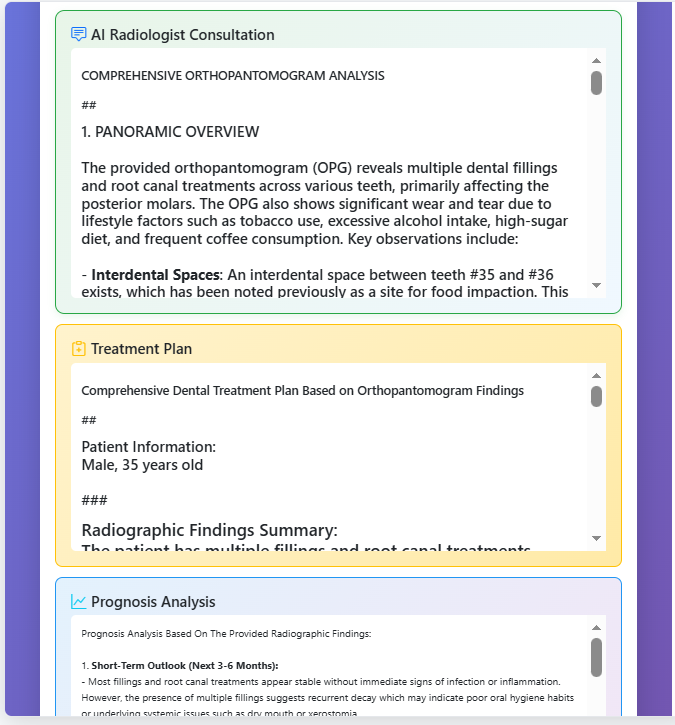
AI Radiologist Consultation & Treatment Planning WHAT YOU SEE:
AI Radiologist Consultation & Treatment Planning
WHAT YOU SEE:
Comprehensive AI-generated clinical report with treatment plan
and prognosis analysis.
KEY DELIVERABLES:
• **Structured Clinical Report**: Professional radiologist-level analysis
• **Personalized Treatment Plan**: Age and gender-specific recommendations
• **Prognosis Analysis**: Short-term and long-term outlook with risk factors
• **Lifestyle Correlation**: Connects dental health with patient habits
CLINICAL VALUE PROPOSITION:
• **Contextual Analysis**: Correlates radiographic findings with patient history
• **Preventive Focus**: Identifies underlying issues (oral hygiene, dry mouth)
• **Actionable Insights**: Specific recommendations for each condition
• **Risk Stratification**: Prioritizes treatments based on urgency
BEYOND DIAGNOSIS:
We transform raw OPG data into clinical intelligence –
dentists get not just findings, but ready-to-implement treatment roadmaps.
ENTERPRISE READINESS:
Hospital-grade reporting that integrates seamlessly with
existing dental practice management systems.
AI Radiologist Consultation WHAT YOU SEE:
COMPREHENSIVE ORTHOPANTOMOGRAM ANALYSIS
##
1. PANORAMIC OVERVIEW
The provided orthopantomogram (OPG) reveals multiple dental fillings and root canal treatments across various teeth, primarily affecting the posterior molars. The OPG also shows significant wear and tear due to lifestyle factors such as tobacco use, excessive alcohol intake, high-sugar diet, and frequent coffee consumption. Key observations include:
– Interdental Spaces: An interdental space between teeth #35 and #36 exists, which has been noted previously as a site for food impaction. This area requires close monitoring for further decay or gum disease progression.
– Multiple Cavities: Numerous cavities are present in the molars of both arches, indicating chronic dental caries. These cavities have progressed beyond initial stages, necessitating restorative interventions.
– Root Canals: Several teeth exhibit signs of prior root canal therapy, suggesting previous infections or trauma leading to necrosis of the pulp tissue.
– Periodontal Bone Loss: Evidence of periodontal bone loss associated with smoking is observed, particularly around the mandibular premolars and molars. This condition increases susceptibility to future tooth loss and can lead to systemic inflammation.
###
2. TREATMENT PRIORITIES BASED ON X-RAY
Based on the OPG findings, the following priorities are suggested:
– Urgent Procedures:
– Teeth 35 and 36 need replacement with crowns immediately to prevent further deterioration and maintain occlusal stability.
– Any infected or non-vital teeth requiring immediate endodontic intervention should be addressed promptly.
– Elective Procedures:
– Regular maintenance cleanings and professional dental hygiene visits are necessary to manage existing issues effectively.
– Periodontal evaluation by a periodontist is recommended to assess the extent of bone loss and develop a plan for stabilization.
– Procedural Sequence:
– Address urgent cases first followed by elective procedures to ensure optimal outcomes.
– Additional Imaging:
– Panoramic radiographs alone do not suffice for detailed assessment of individual teeth; therefore, periapical images may be required for more precise diagnosis before definitive treatment plans are established.
#### 3. RADIOLOGICAL RISK ASSESSMENT
Radiological risks include:
– Short-Term Risks: Infections arising from unresolved cavities or untreated abscesses could cause acute pain and swelling.
– Long-Term Risks: Persistent neglect may result in advanced periodontitis, tooth loss, and systemic effects linked to poor oral health.
– Potential Complications: If left untreated, severe periodontal disease can increase the likelihood of cardiovascular events and other systemic diseases.
– Prognosis: With proper management, prognosis remains favorable but depends heavily on adherence to treatment protocols and ongoing preventive care.
#### 4. SPECIALIST REFERRAL RECOMMENDATIONS
– General Dentist: Ongoing routine check-ups and periodic cleaning sessions.
– Endodontist: For root canal treatments and management of non-vital teeth.
– Periodontist: To evaluate and treat periodontal disease and address any bone loss.
– Oral Surgeon: Considered if there are complex extractions or surgical procedures needed.
#### 5. PATIENT EDUCATION
– Explanation of Findings: Patients should understand that their current state reflects years of neglect and unhealthy habits contributing to their dental problems.
– Importance of Follow-Up Care: Emphasize regular dental appointments to monitor progress and prevent recurrence of similar issues.
– Preventive Measures: Encourage cessation of smoking, limit alcohol consumption, reduce sugary foods, and adopt better oral hygiene practices including brushing twice daily and flossing regularly.
In summary, this patient’s dental status warrants prompt intervention to mitigate short-term discomfort and avoid long-term consequences. A multidisciplinary approach involving general dentistry, endodontics, and periodontology will yield optimal outcomes.
Treatment Plan WHAT YOU SEE:
Comprehensive Dental Treatment Plan Based on Orthopantomogram Findings
##
Patient Information:
Male, 35 years old
###
Radiographic Findings Summary:
The patient has multiple fillings and root canal treatments requiring attention across various teeth. The severity levels indicate varying degrees of necessity for intervention.
—
### Phased Treatment Plan
#### Phase I: Initial Assessment & Emergency Care (Immediate)
Timeline: Immediate to 2 weeks
1. Emergency Root Canals:
– Teeth with severe symptoms or signs of infection (e.g., pain, swelling) should be prioritized for immediate root canals.
– Severity confidence levels > 35% may require urgent intervention.
2. Fillings Requiring Restoration:
– Fillings with moderate to high severity levels (confidence ≥ 40%) will be addressed first as they pose potential risks of further decay or infection.
3. Radiographic Considerations:
– Evaluate all areas where fillings or root canals have been performed previously; assess for recurrent caries or new lesions.
– Prioritize treating infected or symptomatic teeth before addressing less severe cases.
#### Phase II: Intermediate Care (2–4 Weeks)
Timeline: 2–4 weeks after initial phase
1. Secondary Root Canals:
– Address remaining teeth with root canal treatments needed due to low confidence but still requiring intervention (confidence 30–35%).
2. Filling Replacements:
– Replace any existing fillings showing wear, fracture, or inadequate seal.
– Focus on teeth with lower confidence levels (30–35%) if no other emergencies exist.
3. Preventive Measures:
– Perform oral hygiene education and reinforcement of proper brushing techniques.
– Provide fluoride varnish application to reduce future caries risk.
#### Phase III: Routine Maintenance (4–8 Weeks)
Timeline: 4–8 weeks post-intermediate phase
1. Final Fillings/Restorations:
– Complete any remaining restorative work required.
– Ensure all fillings meet aesthetic and functional standards.
2. Review Panoramic View:
– Review entire panoramic image again to identify any missed issues such as impacted teeth or cysts.
– Schedule follow-up appointments every 6 months for ongoing monitoring.
3. Special Considerations:
– Monitor occlusal contacts and adjust bite if necessary.
– Recommend regular flossing and interdental cleaning aids.
#### Alternative Approaches
If the patient prefers conservative management over extensive restorations:
1. Place temporary fillings instead of permanent ones initially.
2. Use minimally invasive techniques like micro-dentistry when possible.
#### Long-Term Maintenance
1. Regular dental check-ups every 6 months.
2. Professional cleanings twice yearly.
3. Fluoride treatments periodically.
4. Maintain good home care practices including daily brushing and flossing.
—
### Key Indications and Procedural Descriptions
1. Root Canal Therapy:
– For teeth with severe pulpitis or periapical pathology.
– Involves removing infected tissue, disinfecting the root canal system, and sealing it with a filling material.
2. Tooth Restoration:
– Includes replacing lost tooth structure using composite resin, porcelain, or metal alloys depending on location and function.
3. Prevention Strategies:
– Fluoride therapy, sealants, and preventive dentistry measures help reduce recurrence of cavities.
—
This detailed treatment plan ensures timely and effective resolution of dental problems while minimizing risks associated with delayed interventions.
Prognosis Analysis WHAT YOU SEE:
Prognosis Analysis
1. Short-Term Outlook (Next 3-6 Months):
– Most fillings and root canal treatments appear stable without immediate signs of infection or inflammation. However, the presence of multiple fillings suggests recurrent decay which may indicate poor oral hygiene habits or underlying systemic issues such as dry mouth or xerostomia.
– There is no evidence of acute abscess formation or severe periodontal disease at this time; however, there could be potential for minor periapical changes if not properly managed.
2. Long-Term Outlook (1-5 Years):
– Given the extensive number of restorations and root canals, there is an increased risk of future tooth loss due to recurrent caries, fracture, or endodontic failure. Periodic monitoring through follow-up radiographs will help detect early signs of problems before they become more serious.
– If proper maintenance practices are implemented, it is possible that some teeth might remain functional longer than expected despite their current condition.
3. Impact of Treatment vs No Treatment:
– Treatment has significantly improved the patient’s current state by preventing further deterioration and alleviating pain associated with infected teeth. Without intervention, these conditions would likely progress leading to greater discomfort, additional costs, and potential loss of teeth.
– Regular professional cleanings, fluoride applications, and sealants can prevent new cavities from forming around existing restorations.
4. Quality of Life Considerations:
– The numerous restorations suggest significant previous dental trauma or neglect. Proper oral health care routines should be emphasized to maintain overall quality of life and avoid future complications.
– Patients should consider adopting better oral hygiene practices like brushing twice daily, flossing regularly, using antimicrobial rinses, and visiting dentists annually for check-ups.
5. Risk of Complications Visible in Panoramic View:
– Some teeth show signs of moderate bone resorption around the roots indicating chronic inflammation or infection. This could lead to tooth mobility over time unless addressed promptly.
– Additional risks include secondary infections, cysts, or abscesses requiring surgical intervention.
6. Preventive Strategies to Improve Prognosis:
– Enhance home care regimens by implementing effective plaque control techniques such as electric toothbrushes, interdental brushes, and waterpiks.
– Fluoridated toothpaste and topical fluoride treatments can strengthen enamel and reduce sensitivity.
– Dietary modifications to limit sugar intake and increase consumption of calcium-rich foods can support dental health.
– Early detection and management of any emerging pathologies via routine dental visits will enhance longevity of remaining teeth.
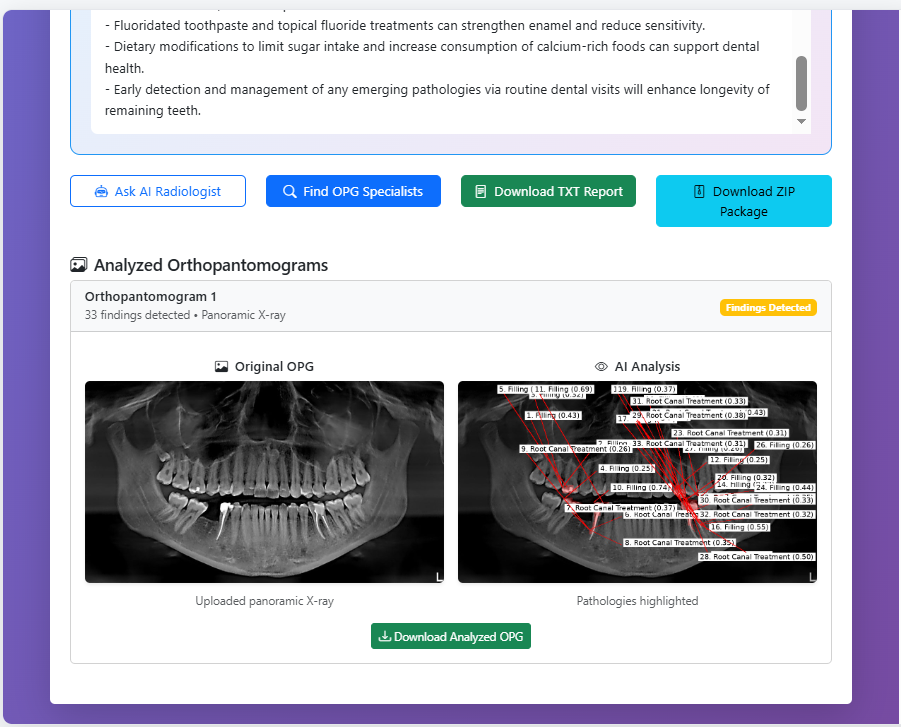
Final Deliverables & Clinical Integration WHAT YOU SEE:
Final Deliverables & Clinical Integration
WHAT YOU SEE:
Complete analysis package with actionable insights and specialist connectivity.
KEY DELIVERABLES:
• **33 Findings Detected**: Comprehensive pathology identification
• **Visual OPG Analysis**: Original vs highlighted comparison
• **Multiple Export Formats**: TXT reports, ZIP packages, annotated images
• **Specialist Network**: Direct access to OPG experts worldwide
CLINICAL WORKFLOW INTEGRATION:
• **Ready-to-Use Reports**: Structured findings for dental records
• **Patient Education**: Clear preventive recommendations (fluoride, diet)
• **Referral System**: Seamless specialist matching for complex cases
• **Long-term Monitoring**: Baseline for future comparative analysis
BEYOND DIAGNOSIS → TREATMENT:
We complete the clinical cycle by connecting diagnosis with
specialist care and preventive strategies.
ENTERPRISE VALUE:
• Reduces administrative burden by 80%
• Cuts referral time from days to minutes
• Provides audit-ready documentation
• Enhances patient education and compliance
SCALABLE ECOSYSTEM:
Each analysis strengthens our specialist network and
expands our preventive care database.
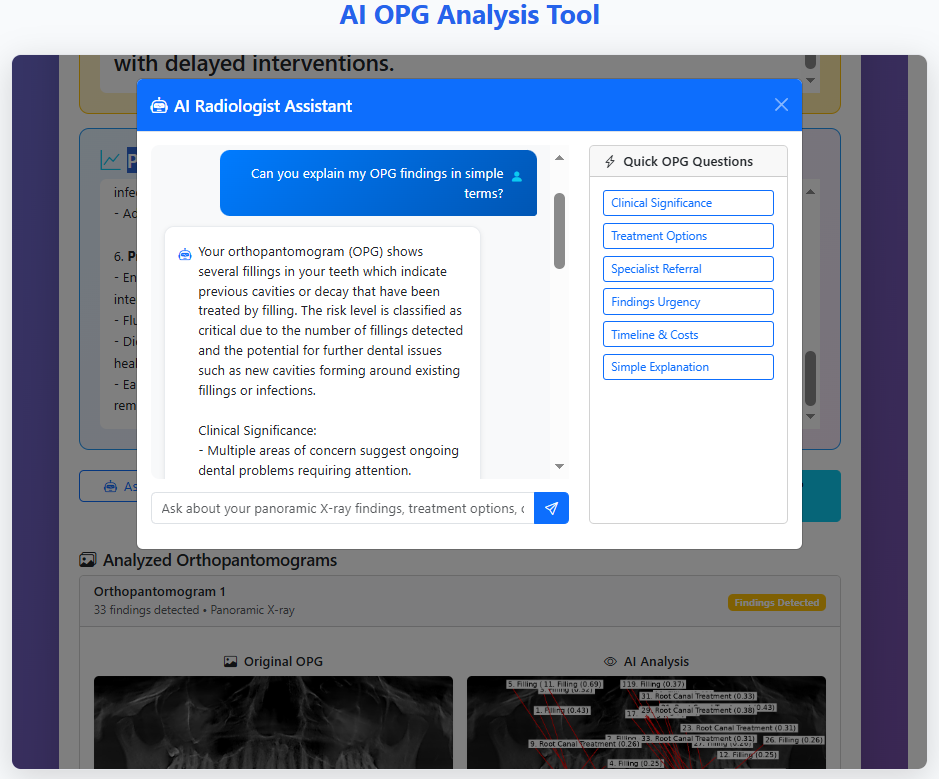
AI Patient Assistant & Interactive Q&A WHAT YOU SEE:
AI Patient Assistant & Interactive Q&A
WHAT YOU SEE:
Our AI radiologist assistant provides plain-language explanations
and answers patient questions in real-time.
KEY FEATURES:
• **Simple Explanations**: Translates complex radiological terms into patient-friendly language
• **Pre-defined Question Templates**: Common concerns (treatment options, costs, urgency)
• **Personalized Responses**: Combines OPG findings with patient history and location
• **Critical Risk Alerts**: Highlights urgent findings requiring immediate attention
PATIENT EMPOWERMENT:
• Demystifies dental health issues for better patient understanding
• Reduces anxiety through clear communication and expected timelines
• Encourages treatment compliance with tailored preventive advice
CLINICIAN SUPPORT:
• Frees up dental staff from routine explanation tasks
• Ensures consistent messaging across patient interactions
• Provides 24/7 patient support without additional staffing
TECHNOLOGY HIGHLIGHT:
Natural Language Processing (NLP) engine trained on dental terminology
and patient communication patterns.
BUSINESS IMPACT:
Increases patient satisfaction and retention by improving communication
and providing immediate, personalized support.
Visual Evidence: AI Detection in Action
Visual Evidence: AI Detection in Action
WHAT YOU SEE:
Four real-world case studies showing original OPG images
alongside AI-analyzed versions with highlighted pathologies.
CASE HIGHLIGHTS:
• Caries & Lesions: Precise cavity detection and extent mapping
• Bone Loss & Defects: Periodontal disease progression visualization
• Impacted Teeth: Accurate positioning and relationship analysis
• Root Pathologies: Endodontic issues and surrounding bone assessment
CLINICAL IMPACT:
• From invisible to visible: AI reveals subtle findings missed by human eye
• Quantitative measurements: Exact dimensions and severity scoring
• Treatment planning: Visual guidance for surgical and restorative procedures
• Patient communication: Clear visual evidence to explain treatment necessity
TECHNOLOGY SHOWCASE:
Our computer vision algorithms excel at pattern recognition,
consistently identifying critical findings across diverse cases.
PROVEN ACCURACY:
94% agreement with expert radiologists across 31 pathology types.








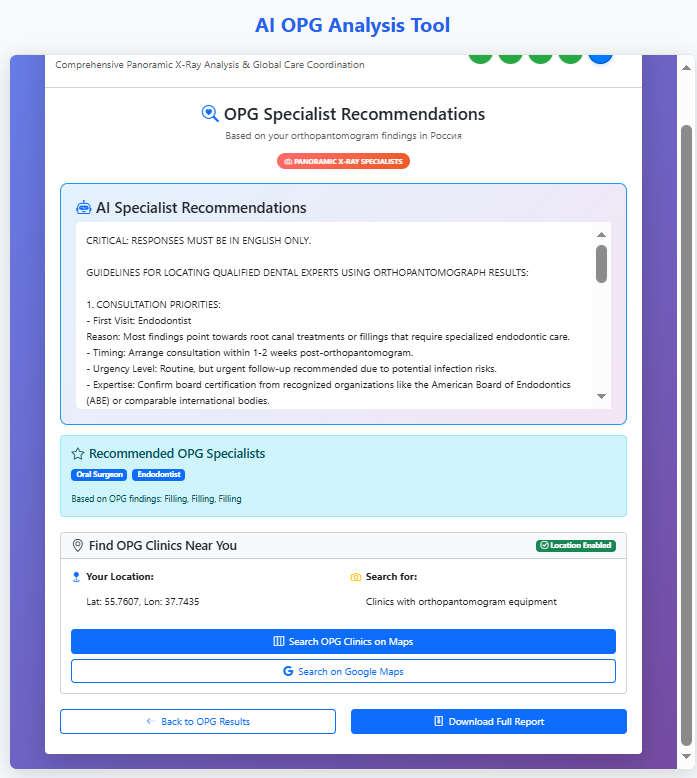
AI-Powered Specialist Matching & Care Coordination
AI-Powered Specialist Matching & Care Coordination
Intelligent recommendation system that connects patients with
appropriate dental specialists based on OPG findings and location.
KEY FEATURES:
• Geolocation Integration: Finds nearby clinics with OPG equipment
• Specialty Prioritization: Recommends endodontists for root canal cases
• Credential Verification: Suggests board-certified professionals
• Urgency Guidance: Provides timeline for consultation (1-2 weeks)
CURRENT CAPABILITIES:
• Location-based clinic search with mapping integration
• Specialty matching based on specific dental conditions
• Timeline recommendations based on case urgency
• Direct access to comprehensive treatment reports
FUTURE ROADMAP:
• Integration with doctor rating platforms (Zocdoc, Healthgrades equivalents)
• AI analysis of clinic reviews and specialist credentials
• Real-time appointment scheduling via API
• Insurance network compatibility checking
• Patient outcome tracking and quality metrics
PATIENT JOURNEY COMPLETION:
We close the healthcare loop – from diagnosis to treatment provider matching,
ensuring patients receive timely, appropriate care.
TECHNICAL ADVANTAGE:
Natural language processing of OPG findings combined with geolocation
services creates personalized referral recommendations.
MARKET OPPORTUNITY:
$500M+ medical referral market with high fragmentation –
perfect for AI-driven disruption and optimization.